RPM Policy Shifts Bring ACO Execution Into Focus

Equipo RPM integrates remote monitoring, care workflows, and billing support, helping ACOs operationalize new CMS RPM rules at scale.
CMS RPM updates expand access for smaller providers, but success now depends on consistent execution across ACO networks.
Equipo RPM platform, which combines remote monitoring, care coordination workflows, and updated billing logic, is increasingly viewed as critical infrastructure in this new environment. As reimbursement rules better align with real-world care delivery, the ability to execute RPM consistently and compliantly becomes just as important as the policy change itself.
RPM has long fit neatly into the theory of population health. Continuous monitoring and early intervention align with cost containment and quality improvement goals. In practice, however, adoption has been uneven. Prior reimbursement rules favored large health systems with dedicated staff and predictable patient engagement. Smaller practices, FQHCs, and rural clinics often delivered RPM-related care without reliable reimbursement, limiting scale and sustainability.
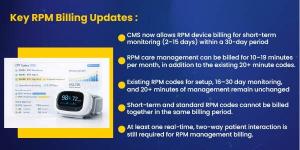
CMS’s updated RPM reimbursement structure reflects how care is actually delivered in these settings. Shorter monitoring periods and shorter, clinically meaningful interactions are now reimbursable. This change lowers the financial risk of participation, but it also introduces new operational complexity. Providers must accurately track monitoring days, engagement thresholds, time spent, and documentation requirements. Without the right systems in place, these gains can be difficult to realize.
For ACOs, the implications are structural rather than financial. ACO performance depends on consistent execution across diverse provider networks. When RPM adoption is fragmented, care models vary and performance leakage increases. Care management platforms help standardize workflows across independent practices, rural clinics, and FQHCs, enabling RPM to function as a network-wide capability rather than a siloed program.
The impact is particularly evident among high-risk patients. These patients often drive emergency department utilization and readmissions, yet they are also the least predictable in terms of engagement. Under previous rules, intermittent participation often made RPM financially impractical. The updated reimbursement framework allows RPM to be used for transitional care, episodic monitoring, and unstable chronic conditions, use cases where early signals matter most.
Here, the role of an integrated platform becomes essential. RPM data alone does not change outcomes. Equipo RPM converts patient readings into actionable workflows by triggering timely outreach, escalating care when clinically appropriate, and documenting activity to support both clinical decision-making and billing compliance. This integration ensures that shorter interactions, now reimbursable under CMS rules, are captured accurately and aligned with each patient’s care plan.
For FQHCs and rural clinics, sustainability is the primary benefit. RPM is unlikely to become a revenue generator, but it can now function as a supported extension of care coordination rather than an unfunded obligation. Care management platforms reduce administrative burden by embedding billing logic, automating documentation, and aligning RPM activity with broader population health workflows. This is particularly important in resource-constrained environments where staffing flexibility is limited.
It is important to remain realistic. These changes do not increase ACO benchmarks or guarantee shared savings. RPM remains a supporting tool, not a standalone strategy. The value emerges when RPM is embedded into care management, quality improvement, and utilization management efforts—areas where execution, not policy, is often the limiting factor.
As CMS lowers participation barriers, platforms like Equipo RPM enable providers to translate policy flexibility into operational consistency. By integrating RPM data, care workflows, analytics, and billing support into a single system, care teams can act earlier, document accurately, and scale programs across diverse provider networks.
The policy update is incremental. The operational impact, when paired with the right infrastructure, is not.
About Equipo RPM
Equipo RPM is part of the Equipo CRM, built to help ACOs, FQHCs, and value-based care organizations run population health programs at scale. Rather than treating RPM as a standalone tool, Equipo embeds it directly into day-to-day care management workflows.
Within Equipo CRM, RPM data flows into a single patient view alongside risk scores, care gaps, quality measures, and utilization history. Care teams can see which patients need attention, why they need it, and what action to take next, without switching systems. RPM alerts trigger structured workflows such as nurse outreach, medication review, post-discharge follow-ups, or escalation to a provider when needed.
The platform also guides teams through RPM documentation and time tracking in line with updated CMS billing rules. Short monitoring periods and shorter clinical interactions are captured automatically within the workflow, reducing missed reimbursement and compliance risk. This is especially valuable for smaller and rural clinics that lack dedicated billing or compliance staff.
By integrating RPM, care management, analytics, and billing support into one platform, Equipo enables consistent execution across diverse provider networks with minimal workflow disruptions.
PRINCE MAMMAN
Equipo Health Inc
+1 732-221-1050
email us here
Visit us on social media:
LinkedIn
Instagram
Facebook
Legal Disclaimer:
EIN Presswire provides this news content "as is" without warranty of any kind. We do not accept any responsibility or liability for the accuracy, content, images, videos, licenses, completeness, legality, or reliability of the information contained in this article. If you have any complaints or copyright issues related to this article, kindly contact the author above.